There are complex congenital cardiopathies that require hybrid management of percutaneous procedures to facilitate or complete surgical outcomes. They are medical-surgical programmes that can be fundamental when planning the therapeutic strategy for such cardiopathies in the long term.
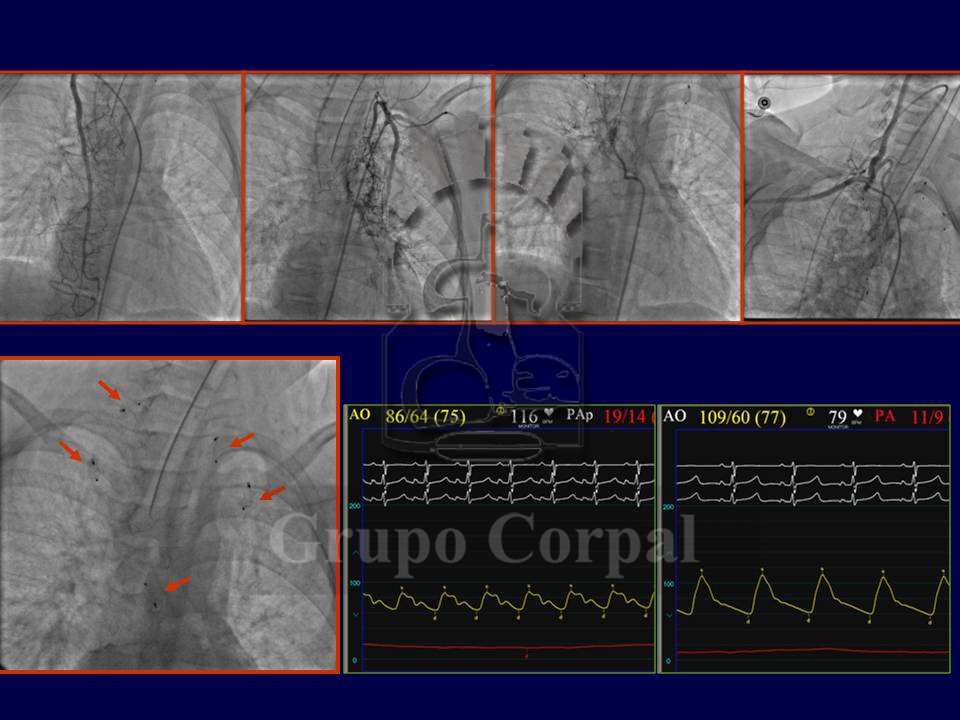
The most common are based on cardiopathies involving a “single ventricle” heart that had to be prepared for a Fontan surgery (connecting the vena cavas with the pulmonary artery) Before that indication we have to maintain an appropriate pulmonary flow without exceeding a pressure value that could prevent such a connection. This is a complex situation, requiring precision in prior palliative measures. Moreover, despite such precision, the bodies of children with marked pulmonary ischaemia develop systemic-pulmonary collateral systems that increase pulmonary flow and could be harmful immediately post-op if they are not first occluded percutaneously (Figure).
Also, if pulmonary pressure is as high as is advisable, during the procedure the surgeon can make fenestrations in the inter-atrial patch, relieving this pressure after the surgery until the heart and circulation adapt to the new situation. When this occurs, percutaneous closure is also required, as in the long term this generates oxygen desaturation in the systemic circulation, solved with the closure (Figure).
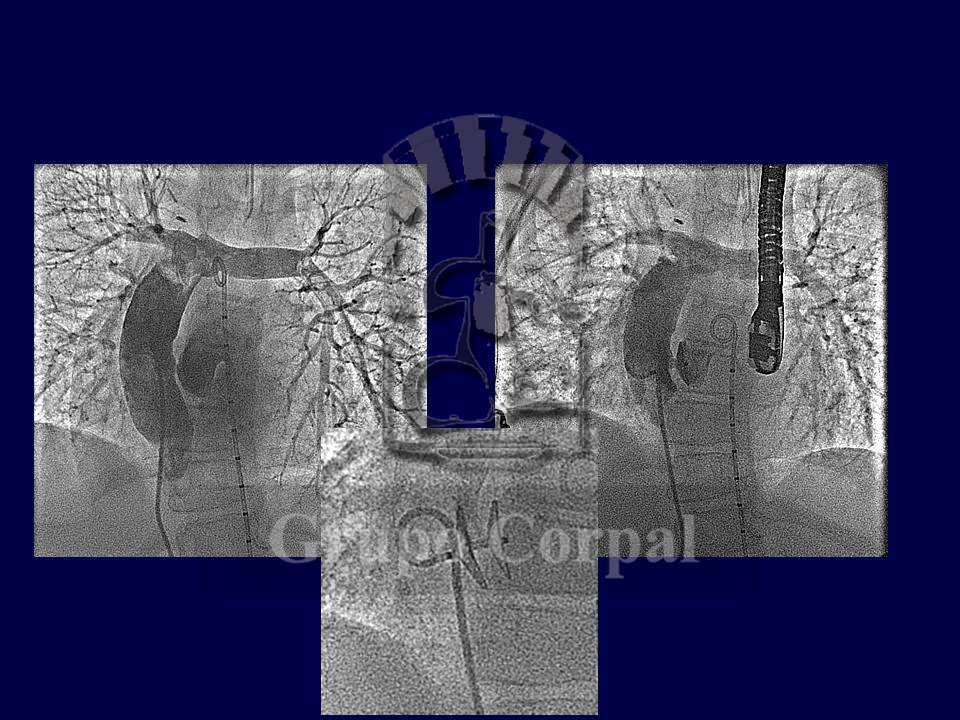
The medical-surgical decision to plan surgeries in the long term to obtain a functioning single-ventricle heart or the development of a hypoplastic ventricle, make it grow into a two-ventricle heart can be complex. Interdisciplinary decisions are required to choose the best route in each case. In patients with pulmonary atresia, a whole interventricular septum and hypoplastic right ventricle, the initial plan starting with a surgical systemic-pulmonary fistula can change if extreme hypoxia persists despite the fistula and it is decided to percutaneously perforate the atresia.
This perforation causes anterograde flow in the right ventricle (albeit poor), together with pulmonary regurgitation, making the right ventricle grow. Over time, the right ventricle can become competent, and the atrial septal defect can be closed (as it also generates systemic oxygen desaturation that has to be corrected) (Figure), thus completing a series of medical-surgical measures that can end in a functioning heart with 2 independent ventricles. Ultimately, only a well-oiled team can successfully complete the treatment of such complex and serious cardiopathies (References).