
Mitral valvuloplasty
Mitral stenosis is a rheumatic disease affecting the anterior and posterior leaflets of the mitral valve, narrowing its orifices and causing mechanical difficulty for filling the left ventricle. This increases the fill pressure in the left atrium, which is hydrostatically transmitted to the pulmonary veins and pulmonary capillary wedge, involving the possibility of interstitial oedema.
This leads to breathing difficulties, with progressing dyspnoea and, in severe cases, acute pulmonary oedema. Besides medical treatment, which can relieve the symptoms, the classic mechanical treatment is mitral valvuloplasty.
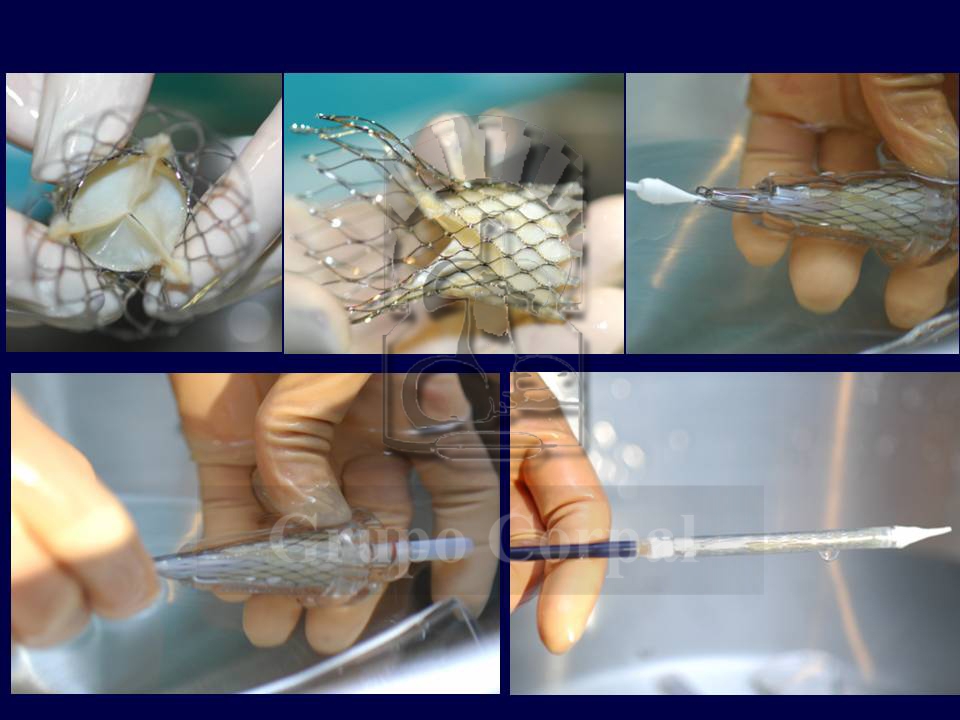
Transcatheter aortic valve implantation (TAVI)
The need for aortic valve replacement was covered from the 1970s by open-heart surgery with extracorporeal circulation in which the sick valve was resected and replaced by an artificial valve stitched to the aortic fibrous ring.
The first valves were metal and long-lasting but required lifelong anticoagulation. Then biological valves started to be implanted, especially in elderly patients, made of avascular swine or pericardial tissue, which required less antithrombotic medication.
Treatment of mitral insufficiency
The prevalence of mitral valve insufficiency increases with age, and the degenerative processes that begin from age 60 make it more common. The incidence of this condition is increasing in the population and, when moderate or severe, it generates serious problems, with regular hospital admissions for heart failure.
Rheumatic causes were the most common in Spain in the past, but they now only represent 20% of the total, as functional and degenerative causes are more common. In the US, only 2% of the 30000 patients diagnosed every year undergo valve replacement surgery.
Closure of peri-prosthetic leaks
The surgical implantation of metal and biological valve replacements requires their suture to the ring of the resected valve. Occasionally, because the ring is either weak or calcified, one of these sutures can open, causing a high-speed peri-prosthetic regurgitation leak, which can lead to haemolysis. If the leak is significant, it can also cause peri-valvular insufficiency that could also lead to heart failure. If the symptoms are important, the need for surgery to suture the leak can be contemplated, as can a new valve replacement if dehiscence is significant.
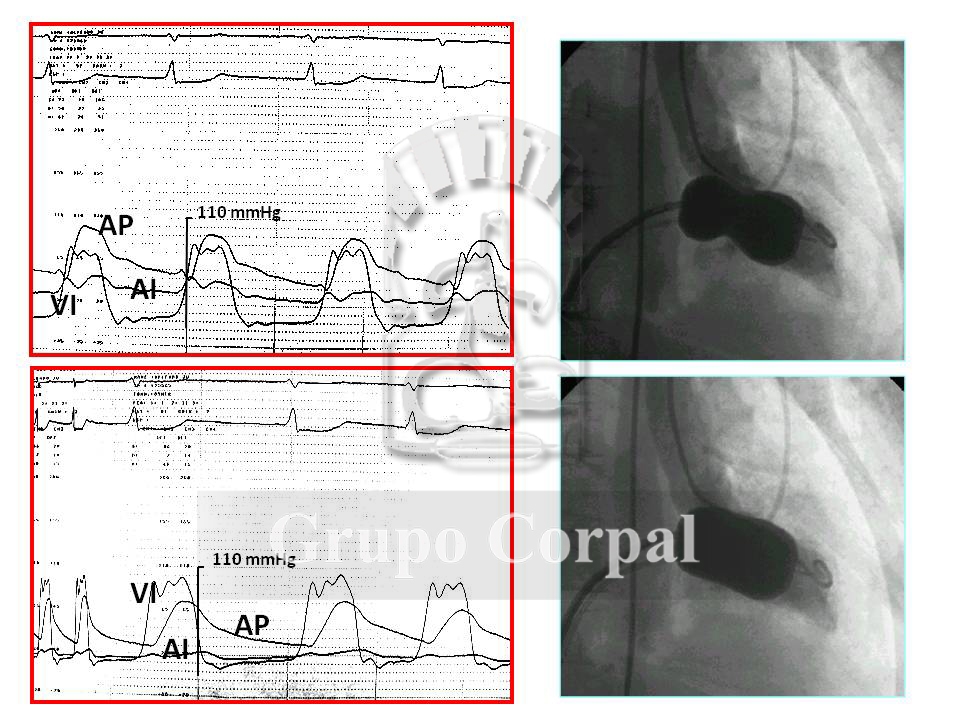
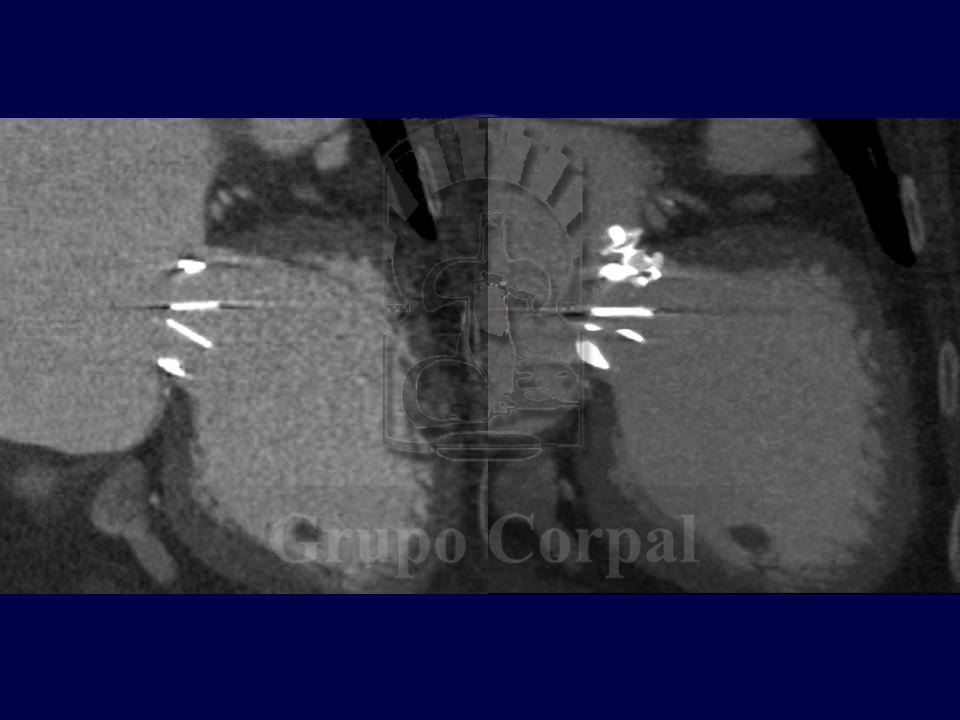
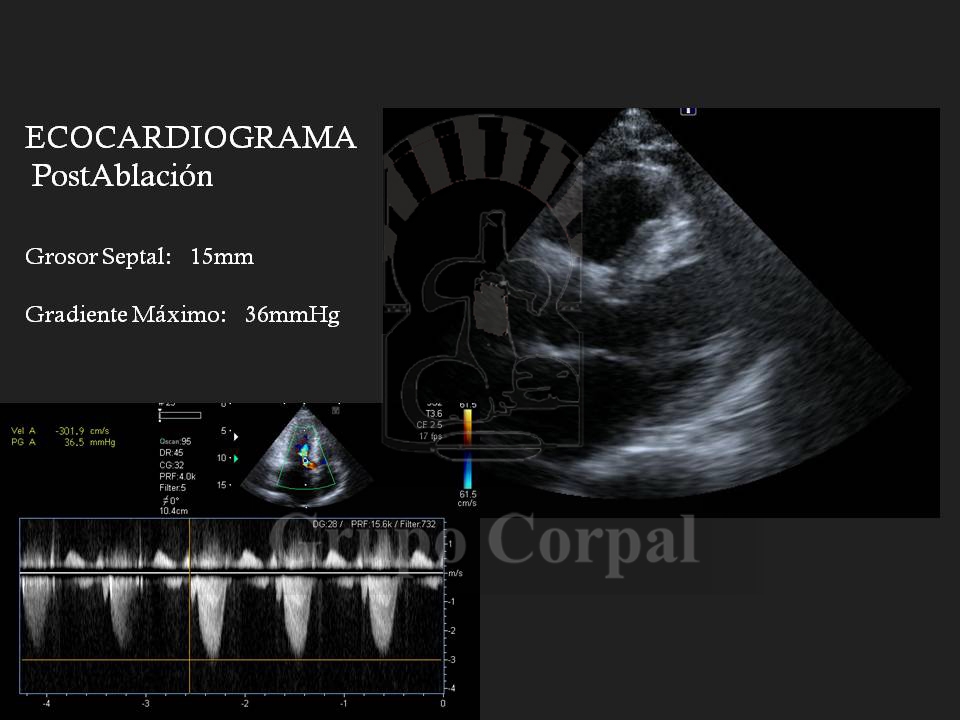
Selective alcohol septal ablation for the treatment of hypertrophic obstructive cardiomyopathy
Hypertrophic Obstructive Cardiomyopathy (HOCM) is a serious cardiomyopathy that is very difficult to treat. It can be progressive, present without a genetic component or be transmitted genetically. The physiopathological base consists of asymmetric hypertrophy with disarrangement of fibres, primarily in the interventricular septum, that dynamically obstructs the outflow of the left ventricle;
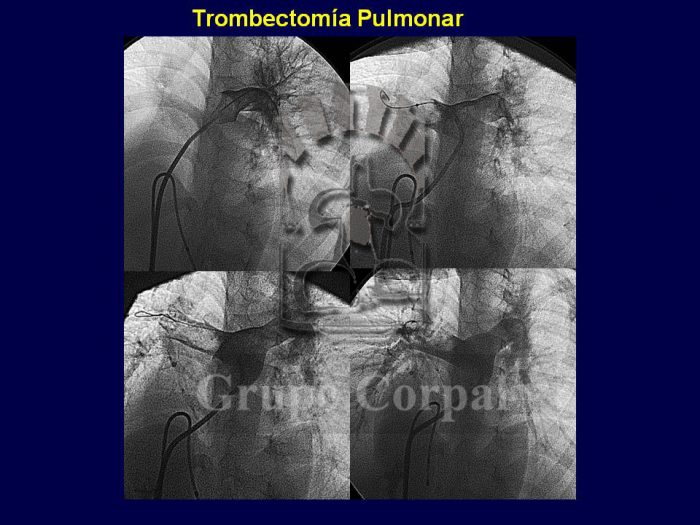
Thrombectomy in acute pulmonary embolism
Clot formation in the venous system is common in people with reduced mobility or bed rest, and in patients who undergo surgery, largely for trauma processes. These silent venous clots, or thrombi, can lead to acute pulmonary embolism, a serious condition capable of causing chest pain, sudden onset dyspnoea and intense systemic desaturation. Massive acute pulmonary embolism can be fatal.
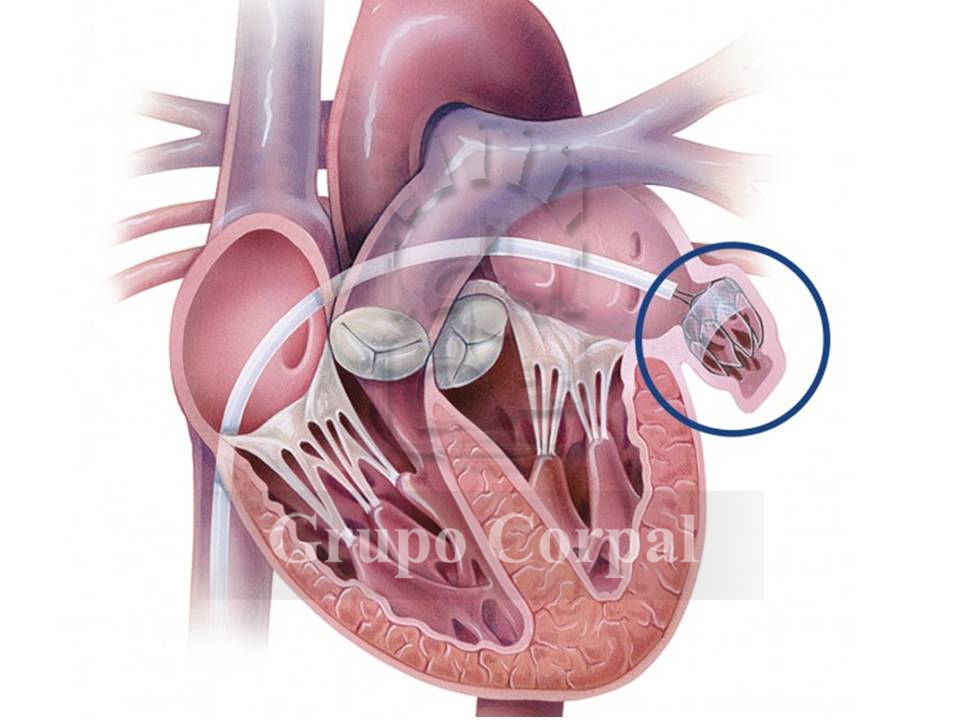
Left atrial appendage closure to prevent systemic embolism in chronic atrial fibrillation
Atrial fibrillation is one of the most common disorders and, in view of the increasing age of the population, its incidence can be expected to grow in the future. The most important complication is systemic embolism, as a result of blood collecting in the left atrium and, in particular, in the left appendage. One way of preventing such embolic episodes is oral anticoagulation.


